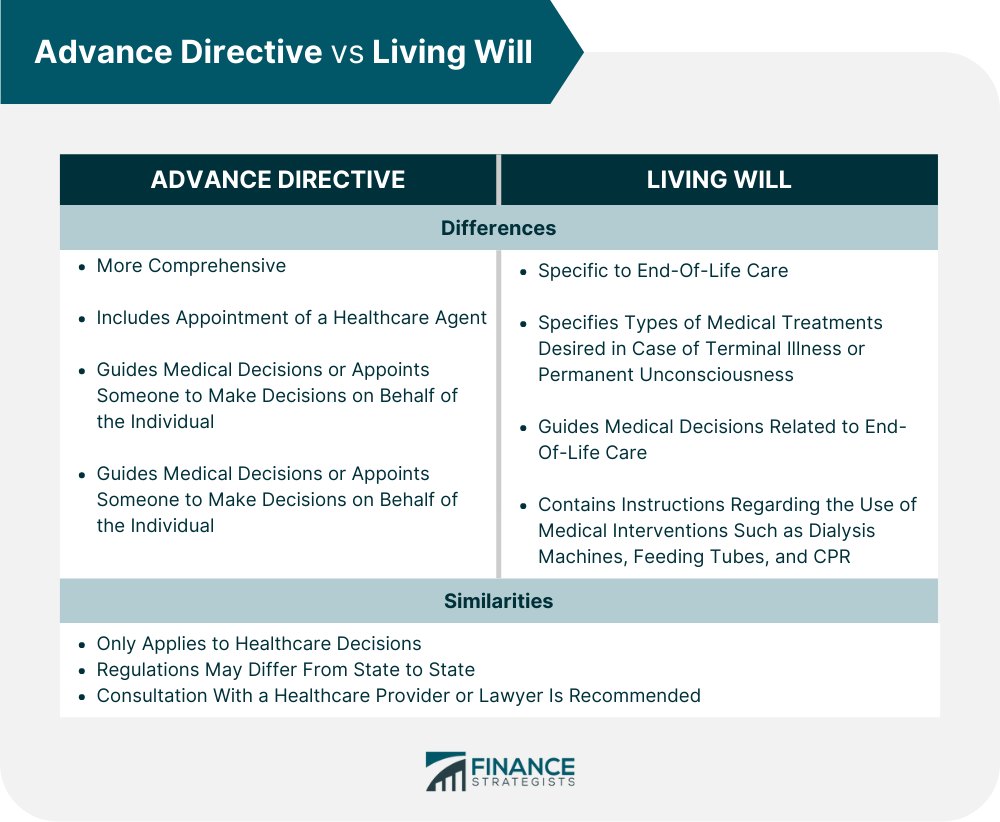
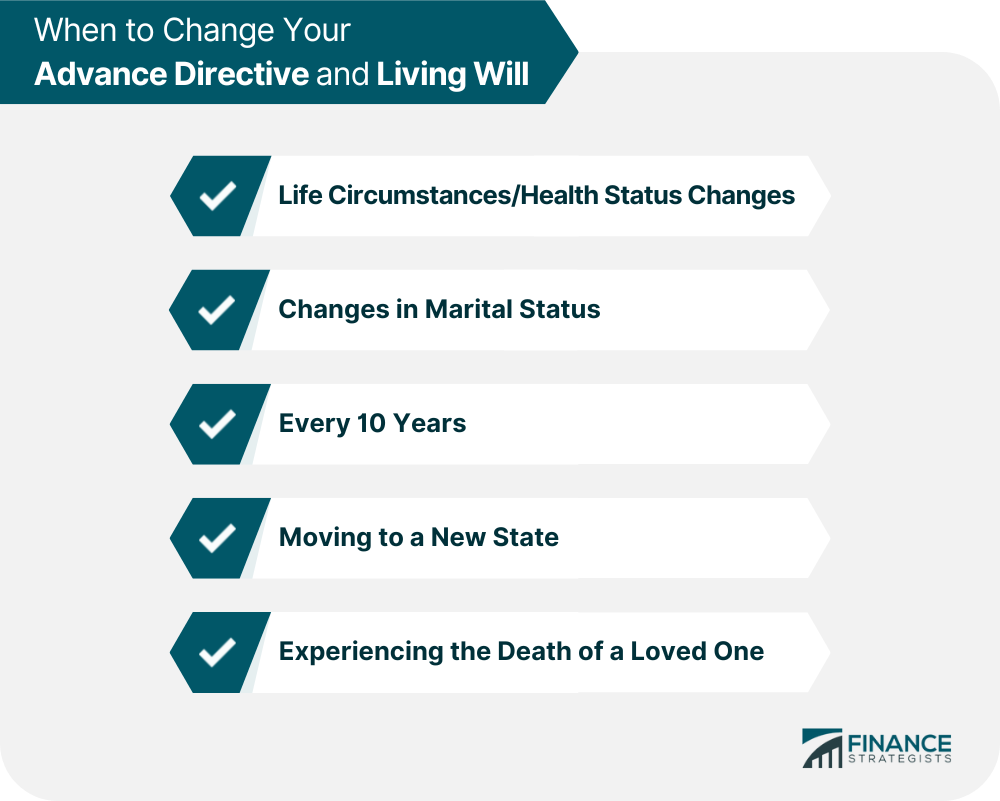
Advance directives and living wills are important documents that help individuals plan and make decisions about their healthcare if they cannot communicate their wishes due to illness, injury, or incapacity. These documents guide healthcare providers and family members regarding the types of medical treatments and procedures an individual would like to receive or avoid. While both advance directives and living will serve similar purposes, there are some key differences between the two documents. Advance directives are more comprehensive and can include the appointment of a healthcare agent and instructions for medical care in addition to end-of-life care. Living wills, on the other hand, are more specific to end-of-life care. An advance directive is a legal document that details the preferred medical decisions of an individual in situations where they cannot make decisions themselves. The document serves as guidance for healthcare providers and loved ones in making medical decisions or appointing someone to make decisions on behalf of the individual. These decisions may pertain to emergency care or special actions required from healthcare providers. Advance directives facilitate individuals to consider and plan their healthcare needs in advance. It is important to note that advance directives only apply to healthcare decisions and not financial or monetary matters, and the regulations surrounding them may differ from state to state. It is recommended that individuals consult with their healthcare provider or lawyer to complete an advance directive when they are in good health so that it may be used if needed in the future when they cannot make medical decisions for themselves. Creating advance directives is an important process that involves documenting the wishes of an individual regarding medical care. This involves writing down the directives in a legal document that needs to be in compliance with state-specific requirements. Although it is not always necessary to ask for legal help, an individual can seek guidance from organizations like the American Bar Association, the National Hospice and Palliative Care Organization, and the AARP, which provides links to state-specific forms. Properly managing and communicating advance directives is crucial to ensure the medical wishes of the individual are followed. Here are some important steps to take: Carry a wallet-sized card indicating they have advance directives Identify their healthcare agent Take note of where a copy of their directives can be found Keep a copy of their advance directives with them when traveling Speak to family members and other important people about their advance directives and healthcare wishes Keep a record of who has their advance directives, including their doctor, health care agent, and any alternate agents Store their original advanced directives in a safe but easily accessible place A living will is an advance directive specifying the particular medical treatment an individual wants to receive if they become unable to make medical decisions due to a terminal illness or permanent unconsciousness. The living will generally contain instructions regarding the use of certain medical interventions to assist in prolonging the life of an individual, such as dialysis machines for kidneys, breathing tubes, feeding tubes, and CPR. The laws pertaining to living wills in the United States may differ depending on the state, and some states may not permit them. To create a living will, the first step is to consider preferred treatment options, such as life-sustaining treatments, medications, surgeries, and end-of-life wishes like organ donation or religious rituals. It is also important to consider appointing a medical power of attorney (POA) to make decisions if the individual cannot communicate their wishes. An individual should obtain a living will form specific to their state. While many states provide free blank forms, online templates often offer customizable frameworks for creating a living will and medical POA. After obtaining a form, the individual should fill it out with their preferences, sign it, and notarize it according to state laws. Most states require two witnesses to a living will, and some require notarization. The individual should store their living will in a safe place and give copies to their healthcare agent, doctor, and the local hospital. It is imperative to revisit the living will periodically, especially as the individual ages or experiences significant life changes, to ensure it continues to reflect their preferences and instructions. Individuals can change their advance directive or living will by creating a new form, distributing new copies, and destroying old ones. However, the requirements for changing directives may vary by state. It is crucial to ensure that a new directive replaces the old one in medical files and charts. Individuals should also discuss changes with their primary care doctor, healthcare agent, family, and friends. Life circumstances or health status changes may necessitate updates to a living will. For example, a terminal diagnosis or a diagnosis that significantly alters the life of an individual may require a reevaluation of their medical preferences. It is essential to consult with a doctor about the treatment options and care decisions that may be required during the course of the disease. Changes in marital status, such as getting married, divorced, separated, or widowed, may also require a revision of a living will, especially when choosing a new healthcare agent. It is recommended to review a living will about every ten years or as life circumstances change to ensure that it reflects the current values and wishes of the individual about end-of-life care. Regularly revisiting a living will help make updates and changes as necessary. Individuals should update their living will in response to changes in medical technology, healthcare laws, health, finances, or beliefs concerning end-of-life care. It is also important to update a living will if a different person is designated to make healthcare decisions, if they move to a new state, or experience the death of a loved one. Remember, executing a new living will revoke the previous one. Advance directives and living will offer various advantages, such as ensuring that the medical care preferences of an individual are respected, especially when they become incapacitated. Some of the benefits are: Providing a comprehensive plan for medical decision-making that works together to address all possible scenarios. Including a medical power of attorney that allows the appointment of a trusted individual to make decisions on behalf of the individual. Addressing preferences for future mental health treatment through the inclusion of psychiatric advance directives. Forcing individuals to think about important questions regarding their medical care preferences. Offering peace of mind for individuals, knowing that their wishes will be honored. Helping family members navigate a difficult time with confidence in accepting or declining treatments from healthcare providers. Advance directives and living wills are essential legal documents that help individuals plan and make decisions about their healthcare. They provide guidance to healthcare providers and loved ones regarding the types of medical treatments and procedures an individual would like to receive or avoid. Creating and communicating these documents is a crucial step in ensuring that the medical care preferences of an individual are respected. It is recommended that individuals consult with their healthcare provider or lawyer to complete an advance directive when they are in good health. If you have not created an advance directive or living will yet, take action now to ensure your medical care preferences are documented and communicated. Consult with your healthcare provider or estate planning lawyer to complete an advance directive and living will, and make sure to properly manage and communicate your directives to those who need to know.Advance Directive vs Living Will: Overview
What Is an Advance Directive?
Creating an Advance Directive
What Is a Living Will?
Creating a Living Will
When to Change Your Advance Directive and Living Will
Benefits of Having a Living Will & an Advance Directive
Final Thoughts
Advance Directive vs Living Will FAQs
An advance directive is a legal document that details the preferred medical decisions of an individual in situations where they are unable to make decisions themselves due to illness, injury, or incapacity. This document serves as guidance for healthcare providers and loved ones in making medical decisions or appointing someone to make decisions on behalf of the individual.
A living will is a type of advance directive that specifies the particular medical treatment an individual wants to receive if they become unable to make medical decisions due to a terminal illness or permanent unconsciousness. The living will generally contain instructions regarding the use of certain medical interventions to assist in prolonging the life of an individual, such as dialysis machines for kidneys, breathing tubes, feeding tubes, and CPR.
While both advance directives and living will serve similar purposes of helping individuals plan and make decisions about their healthcare, there are some key differences between the two documents. Advance directives are more comprehensive and can include the appointment of a healthcare agent and instructions for medical care in addition to end-of-life care. Living wills, on the other hand, are more specific to end-of-life care and do not typically include instructions for other medical care.
Yes, it is possible to have both an advance directive and a living will.
While it is not required to have an attorney create an advance directive or living will, it is recommended to consult with an attorney, healthcare provider, or other legal professionals to ensure the document is legally valid and accurately reflects the wishes of an individual.
True Tamplin is a published author, public speaker, CEO of UpDigital, and founder of Finance Strategists.
True is a Certified Educator in Personal Finance (CEPF®), author of The Handy Financial Ratios Guide, a member of the Society for Advancing Business Editing and Writing, contributes to his financial education site, Finance Strategists, and has spoken to various financial communities such as the CFA Institute, as well as university students like his Alma mater, Biola University, where he received a bachelor of science in business and data analytics.
To learn more about True, visit his personal website or view his author profiles on Amazon, Nasdaq and Forbes.















